Latest News
Research
Abundance of iron drives cell death and could be key to development of novel treatments for neuroblastoma
Feb 19, 2021
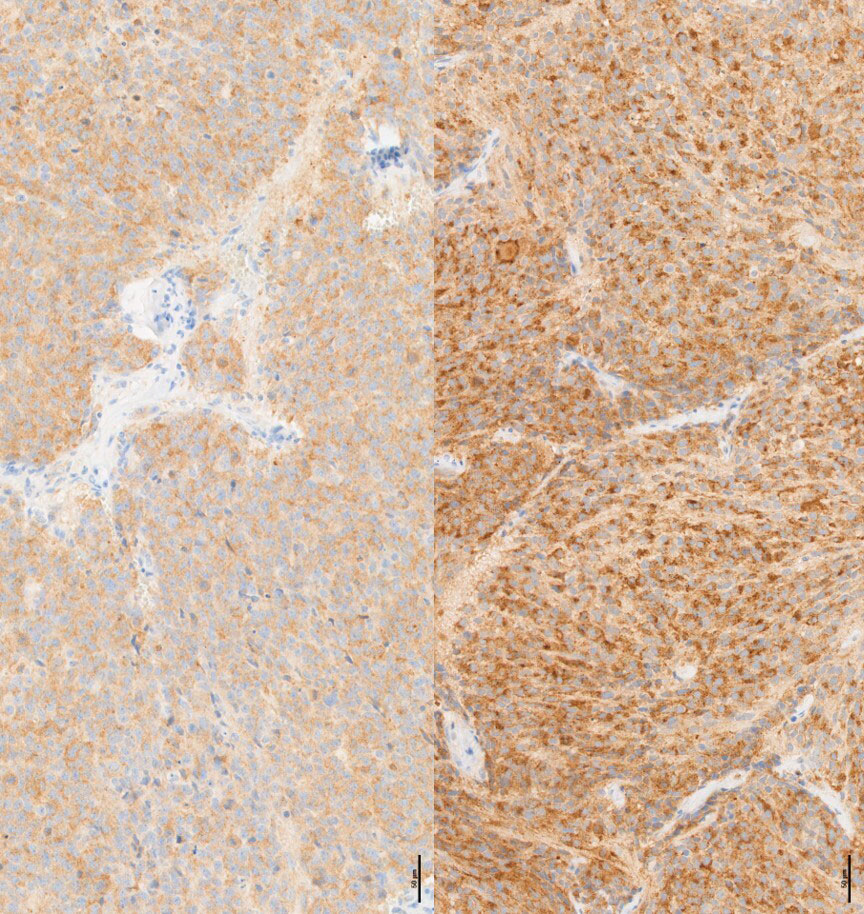 This image shows expression of a specific ferroptosis marker called TfR1 in MYCN-amplified neuroblastoma tissues before and after treatment with auranofin, an FDA-approved drug for rheumatoid arthritis.
This image shows expression of a specific ferroptosis marker called TfR1 in MYCN-amplified neuroblastoma tissues before and after treatment with auranofin, an FDA-approved drug for rheumatoid arthritis.
Neuroblastoma is a cancer that develops in nerve tissue, most commonly in the glands around the kidneys. The gene MYCN is overexpressed in 20-25% of neuroblastoma, and MYCN-amplified neuroblastoma contributes to a considerable percentage of pediatric cancer-related deaths.
Anthony Faber, Ph.D., and a team of researchers at VCU Massey Cancer Center were awarded a grant from the American Cancer Society to study how MYCN and an abundance of iron can drive cancer cell death in neuroblastoma and potentially be targeted with novel treatments. This award is the first part of a potential two-stage grant worth a combined total of $600,000.
“Iron is a double-edged sword in a cancer cell. It can help the cancer grow and survive, but it also creates these toxic molecules within the cell called reactive oxygen species,” said Faber, Natalie N. and John R. Congdon Chair in Cancer Research and co-leader of the Developmental Therapeutics research program at Massey and associate professor in the Philips Institute for Oral Health Research at the VCU School of Dentistry.
Reactive oxygen species (ROS) are highly unstable chemical molecules that react with other molecules within a cell and cause damage to genes and cell death (ferroptosis). Ferroptosis is a recently discovered type of cell death that is largely influenced by the accumulation of iron. Faber said there is a relatively small scientific understanding of ferroptosis, and even less is known about which cancers may be prone to ferroptosis-inducing drugs.
Through recent research published in Cancer Research, Faber and his collaborators have determined that the MYCN gene creates a vulnerability to drugs that induce ferroptosis because MYCN uses a lot of iron to help power the cancer cell and grow uncontrollably.
By ramping up the systems that remove toxins on a cellular level, MYCN generates so much iron that it also initiates a weakness to drugs that block the ability of the cell to eliminate ROS, as discovered by Konstantinos Floros, Ph.D., postdoctoral fellow at Massey and the Philips Institute for Oral Health Research whose extensive background in cell death effectively advanced this research project.
The researchers found that blocking these detoxifying systems with available drugs makes MYCN-amplified cells sick and die.
“As MYCN continues to be one of the most important targets in cancer therapeutics, this study highlights a new and clinically important strategy for treating MYCN-associated cancers,” Faber said.
Using preclinical tumor models, Faber’s team will use the grant funding to test the ability of sulfasalazine and auronofin – drugs FDA-approved for rheumatoid arthritis – to induce ferroptosis and tumor responses in neuroblastoma cells with high levels of MYCN.
“Fortunately, the Cancer Mouse Models Core run by Jennifer Koblinski, Ph.D., and Bin Hu, Ph.D., at Massey is spectacular and will allow us to robustly test these FDA-approved drugs in both patient-derived models and orthotopic models, where the tumors grow atop the adrenal glands similar to the way they grow in patients,” Faber said.
Faber said that if they show positive results testing these drugs in cancer models, then they can confidently test these therapies in clinical trials.
“This Mission Boost Grant from the American Cancer Society allows us to conduct one of the earliest studies to link a cancer-driving gene to ferroptosis,” Faber said. “This is a significantly important field of study that may have far-reaching implications in cancers beyond neuroblastoma, including some small cell lung cancers and triple negative breast cancer, which rely on a similar protein (c-MYC) to drive their growth.”
Faber and Floros’ collaborators on the Cancer Research study and ongoing grant funding project include Koblinski and Mikhail Dozmorov, Ph.D., members of the Cancer Biology research program at Massey; Sosipatros Boikos, M.D., member of the Developmental Therapeutics research program at Massey; Benjamin Belvin Ph.D., Carter Fairchild, Colin Coon, Janina Lewis, Ph.D., JingYang Cai Ph.D., Krista Powell M.S., Richard Kurupi and Sheeba Jacob Ph.D., of the VCU Phillips Institute for Oral Health Research; Hu, Madhavi Puchalapalli, M.S., and Mayuri Shende, of the Department of Pathology at the VCU School of Medicine and Massey; Kimberly Swift and Sivapriya Ramamoorthy, Ph.D., of Metabolon, Inc.; and John Glod, M.D., Ph.D., of the NCI Pediatric Oncology Branch.
This published study was supported by a National Cancer Institute award (R01CA215610), an American Cancer Society Mission Boost Grant (MBG-20-133-01-MBG) and an Andrew McDonough B+ Foundation Childhood Cancer Research Grant. Services and products in support of the research project were generated by the VCU Cancer Mouse Models Core laboratory, supported, in part, with funding from Massey’s NIH-NCI Cancer Center Support Grant P30 CA016059.
Written by: Blake Belden
Related News
Research
Massey becomes first U.S. site to enroll patients in global Phase 2a trial of first-in-class therapy for T-cell lymphomaJul 24, 2025
Research
Massey welcomes Venkata Battula, Ph.D., as assistant director of Cancer Research Training and Education Coordination Efforts (CRTEC)Jul 21, 2025

Get access to new, innovative care
Treatments in clinical trials may be more effective or have fewer side effects than the treatments that are currently available. With more than 200 studies for multiple types of cancers and cancer prevention, Massey supports a wide array of clinical trials.

Find a provider
Massey supports hundreds of top cancer specialists serving the needs of our patients. Massey’s medical team provides a wealth of expertise in cancer diagnosis, treatment, prevention and symptom management.